What Is Schizotypal Personality Disorder?
Schizotypal Personality Disorder (STPD) is a mental health condition characterized by social and interpersonal difficulties, eccentric behavior, and unusual thoughts or perceptions.
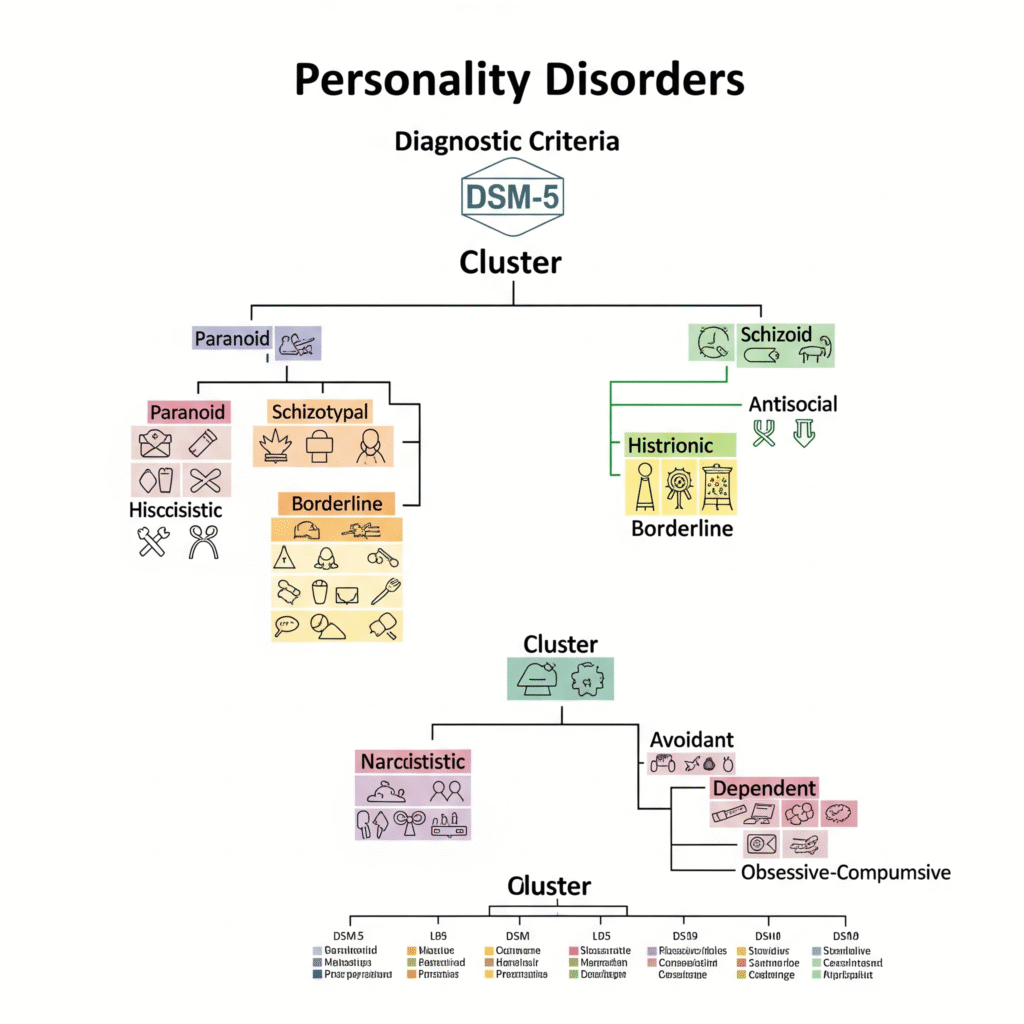
It falls under Cluster A personality disorders in the DSM-5-TR (2022), which are often described as “odd or eccentric.”
While STPD shares some features with schizophrenia, people with schizotypal personality disorder usually do not experience full-blown psychosis, such as persistent hallucinations or delusions.
Approximately 3% of the general population may have schizotypal personality disorder, though it is often underdiagnosed because many people do not seek treatment.
Key Symptoms of Schizotypal Personality Disorder
Symptoms of STPD are diverse but often include:
- Odd beliefs or magical thinking: E.g. believing in telepathy or superstitions
- Unusual perceptual experiences: Feeling that external events carry personal meaning
- Suspiciousness or paranoid thoughts
- Odd thinking or speech: Vague, metaphorical, overly elaborate
- Inappropriate or constricted emotions
- Eccentric appearance or behavior
- Lack of close friends outside of family
- Excessive social anxiety that doesn’t diminish with familiarity
Unlike schizophrenia, individuals with STPD maintain some grasp on reality.
How Schizotypal Personality Disorder Differs from Other Disorders
vs. Schizophrenia
- Schizophrenia often includes persistent hallucinations and delusions, while STPD involves milder, transient psychotic-like experiences.
- People with STPD typically do not lose touch with reality completely.
vs. Schizoid Personality Disorder
- STPD: Has odd beliefs, eccentricity, and social anxiety.
- Schizoid PD: Simply prefers solitude and shows emotional coldness, without odd beliefs.
vs. Social Anxiety Disorder
- In social anxiety disorder, people fear embarrassment or judgment.
- In STPD, social anxiety often stems from suspiciousness or paranoid fears.
Causes and Risk Factors
The exact cause of STPD is unknown, but several factors may contribute:
- Genetics: Higher rates of STPD in relatives of people with schizophrenia.
- Brain differences: Abnormalities in brain regions related to social behavior and thought processing.
- Environmental factors: Childhood neglect, trauma, or early stress may play a role.
STPD is slightly more common in men than in women.
Diagnosis and DSM-5 Criteria
Diagnosis involves:
- Psychiatric interviews
- Evaluation of personal and family mental health history
According to the DSM-5-TR, a person must show at least five of the following:
- Ideas of reference (excluding delusions of reference)
- Odd beliefs or magical thinking
- Unusual perceptual experiences
- Odd thinking and speech
- Suspiciousness or paranoid ideation
- Inappropriate or constricted affect
- Odd or eccentric behavior or appearance
- Lack of close friends or confidants
- Excessive social anxiety
Symptoms must start by early adulthood and persist across various situations.
Treatment for Schizotypal Personality Disorder
Many people with STPD do not seek treatment because they may be unaware their thoughts or behaviors are unusual. However, treatment can help improve functioning.
Psychotherapy
- Cognitive Behavioral Therapy (CBT): Helps challenge odd beliefs and reduce social anxiety.
- Social skills training: Builds confidence in social interactions.
- Supportive therapy: Provides a safe space for discussing experiences and fears.
Medications
While no medications are specifically approved for STPD, doctors may prescribe:
- Low-dose antipsychotics: For transient psychotic symptoms.
- Antidepressants or anti-anxiety medication: If mood or anxiety symptoms are present.
Treatment is tailored to individual needs and co-occurring conditions.
Living with Schizotypal Personality Disorder
People with STPD can lead meaningful lives, especially with:
- Early diagnosis
- Therapy to build social skills and reality testing
- Support networks, including family, friends, or support groups
- Consistent self-care routines
It’s important to remember that STPD is a lifelong condition but symptoms can improve, and many individuals function well, especially in roles that don’t demand frequent social interaction.